Element POC®
Blood Gas & Electrolyte Analyzer
Handheld critical care wherever you need it.
-
Handheld Portability
Chemistry, electrolytes, hematology, acid-base and blood gas results where you need them. Great for serial blood testing.
-
Wireless Data Capture
Wi-Fi and bluetooth compatible for convenient management of patient results. Use easily in-clinic or for field applications.
-
Convenient Touchscreen
Easily enter and review patient data.
-
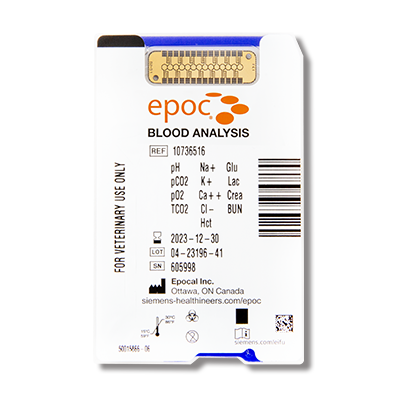
Now With BUN
Complete your renal parameters with the addition of Blood Urea Nitrogen (BUN).
-
Get Results Fast
Accurate critical data in as little as 35 seconds with less than 100 uL of blood.
-
Convenient Test Card
All tests on one test card platform, no refrigeration required, zero warm up time and simplified inventory management.
Rapid, Portable, Wireless Critical Care
Now with BUN!
One Test Card
18 Parameters conveniently on one, room temperature storage card. No warm up period required.
Low Cost Per Test
Increase customer compliance with low cost testing option in critical situations.
Simplified Data Integration
Wi-Fi and Bluetooth capability makes saving a retrieving data easy.
Integrated Calibration
Internal QC checks prior to sample application eliminates redraws.
Built-In Species Reference Ranges
Species specific for Dog, Cat and Horse.
Easy Operation
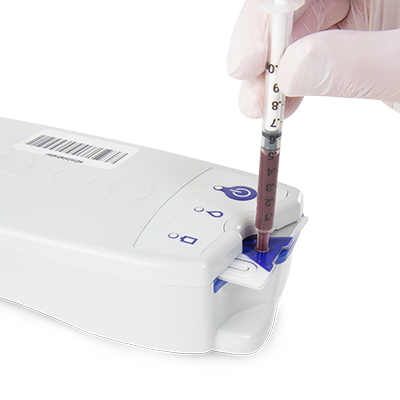
3-Step Measurement. Simply insert test card, fill sample entry port and view results in 35 seconds.
We have used Heska equipment in our emergency practice from the start. Not only is it extremely cost effective, it provides repeatable, accurate results. We trust and depend on it in the middle of the night. The chemistry analyzer makes serial electrolyte checks affordable enough to do, and the Element POC provides solid blood gas information.

Frisco Emergency Pet Care
Estimated Savings 40%
Technical Details & Downloads
Test Menu
Element POC (epoc) provides results 35 seconds after sample introduction. All results are available from a single test card which is stored at room temperature. This represents a significant advantage over other handheld, cartridge-based technologies that require you to choose which parameters you need, or the more expensive alternative of running multiple consumables to get all the parameters that Element POC gives you from one test card.
Measured parameters:
pH, pCO2, pO2, Na+, K+, Cl-, Ca++, Creatinine, BUN, Glucose, Lactate, Hct
Calculated parameters:
cTCO2, cHCO3-, BE (ecf), BE (b), AG, cSO2, cHGB
Species
Element POC has programmed reference ranges for Dog, Cat, and Horse for both venous and arterial samples. Results outside the normal range are flagged. This represents a significant advantage over other handheld, cartridge-based technologies that do not contain species specific reference ranges. All values, including flagged values outside the species specific reference ranges, will transmit via Bluetooth or WiFi to your practice management software (Heska integration required) or epoc wireless printer (sold separately).
Consumable Shelf Life
Element POC test cards have up to 180 days dating from the date of manufacture.
Best-in-Class Technology
Element POC (epoc) utilizes a single-use test card that is stored at room temperature and contains gold electrodes and calibration fluids to calibrate the analyzer prior to each sample analysis. Potentiometric, amperometric and conductometric measurements are utilized to generate all measured parameters. Measured parameters are then utilized to generate calculated parameters. Element POC has a detachable hand-held display (host), and a separate reader that accepts the test card. The two pieces communicate wirelessly via Bluetooth.
Storage Capability
Element POC has 256 MB of built in RAM. This is enough memory to store approximately 3000 separate results. You can also transmit results to your clinic PC and store as many results as your computer storage capacity will hold.
Blood Sample Requirement
A minimum sample volume of at least 92 uL of whole blood from arterial, venous or capillary source is required for analysis. Untreated sample should be analyzed immediately. Lithium, balanced or sodium heparin may be utilized as anticoagulant. Balanced heparin is recommended for the most accurate ionized calcium results. Over dilution of sample with sodium heparin may impact accuracy of sodium results.
Whole blood from arterial, venous or capillary source can be used. A minimum sample volume of at least 92 uL is required for analysis. Untreated whole blood should be analyzed immediately after drawing to obtain most accurate results. Alternatively, lithium, balanced or sodium heparin anti-coagulated whole blood may also be tested. Balanced heparin is recommended for the most accurate ionized calcium results. Over-dilution of sample with sodium heparin may impact accuracy of sodium results.
Calibration
Element POC single use test cards (stored at room temperature) contain calibration fluids to automatically calibrate the analyzer prior to each sample analysis. This process is completed prior to sample introduction which decreases the potential of clotting in the test card and generating errors. This represents a significant advantage over other handheld, cartridge-based technologies that require sample to be introduced prior to the calibration process.
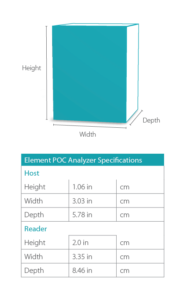
Dimensions
Heska Support Teams are Here for You
We’re Available When You Need Us
Rest assured that when you need help, have questions, or have difficulties, we have you covered.
- Available 6:00am – 5:00pm MST Daily
- Emergency Support During Off-Hours
- Case Consultations or Product Usage Help